Minimally invasive spine surgery (MISS) has revolutionized the treatment of many spinal conditions. Unlike traditional open surgery, which often requires large incisions and significant disruption of muscle and tissue, MISS uses smaller incisions and specialized instruments to access the spine. This approach can lead to less pain, faster recovery, and a quicker return to daily activities. However, not everyone is an ideal candidate for MISS. Understanding who benefits most from this advanced surgical technique is crucial for making informed decisions about your spinal health.
Minimally invasive spine surgery is a broad term encompassing various surgical techniques designed to achieve the same objectives as traditional open surgery but with less disruption to the body. Imagine the spine as a house, and traditional surgery as dismantling a large portion of the roof and walls to gain access to an internal plumbing issue. Minimally invasive surgery, on the other hand, is like using a small access panel and specialized tools to fix the same plumbing, leaving most of the structure intact.
How Does it Differ from Traditional Surgery?
The primary difference lies in the surgical approach. In traditional open surgery, a longer incision is made, and muscles are often cut or retracted extensively to visualize the spine. This can cause significant pain and a longer recovery period due to tissue trauma. MISS, conversely, utilizes smaller incisions, typically less than an inch, and employs techniques such as:
- Tubular Retractors: These small tubes are inserted through the incision, gently pushing muscle tissue aside rather than cutting it. This creates a working channel to the spine.
- Endoscopes/Microscopes: Tiny cameras and powerful microscopes are used to provide the surgeon with a magnified and illuminated view of the surgical area, enabling precise work through small openings.
- Specialized Instruments: Long, thin instruments are designed to work through the small incisions and tubular retractors, performing tasks like removing disc material, decompressing nerves, or stabilizing vertebrae.
This “keyhole” approach aims to minimize damage to healthy tissues, which can translate into several benefits for the patient.
Benefits of Minimally Invasive Surgery
The advantages of MISS compared to traditional open surgery are often significant:
- Smaller Incisions: Leading to less scarring.
- Less Muscle Damage: Muscles are gently moved aside rather than cut, preserving their integrity and function.
- Reduced Blood Loss: Smaller incisions and less tissue disruption generally result in less bleeding during surgery.
- Less Post-Operative Pain: With less tissue trauma, patients typically experience less pain after surgery, often requiring fewer strong pain medications.
- Faster Recovery Time: A quicker return to daily activities and work is a common outcome.
- Shorter Hospital Stays: Many MISS procedures can be performed on an outpatient basis or with a shorter hospital stay.
- Lower Risk of Infection: Smaller incisions can sometimes lead to a reduced risk of incision-related infections.
These benefits make MISS an attractive option for many patients struggling with spinal conditions.
For those considering Minimally Invasive Spine Surgery (MISS), understanding the various options available is crucial in determining the best course of action. A related article that delves into specific procedures is “Cervical Disc Replacement vs. MIS Cervical Foraminotomy: Which is Better?” This resource provides valuable insights into the differences between these two surgical approaches, helping patients make informed decisions about their treatment. To read more about these options, visit the article here: Cervical Disc Replacement vs. MIS Cervical Foraminotomy: Which is Better?.
What Conditions Can Be Treated with MISS?
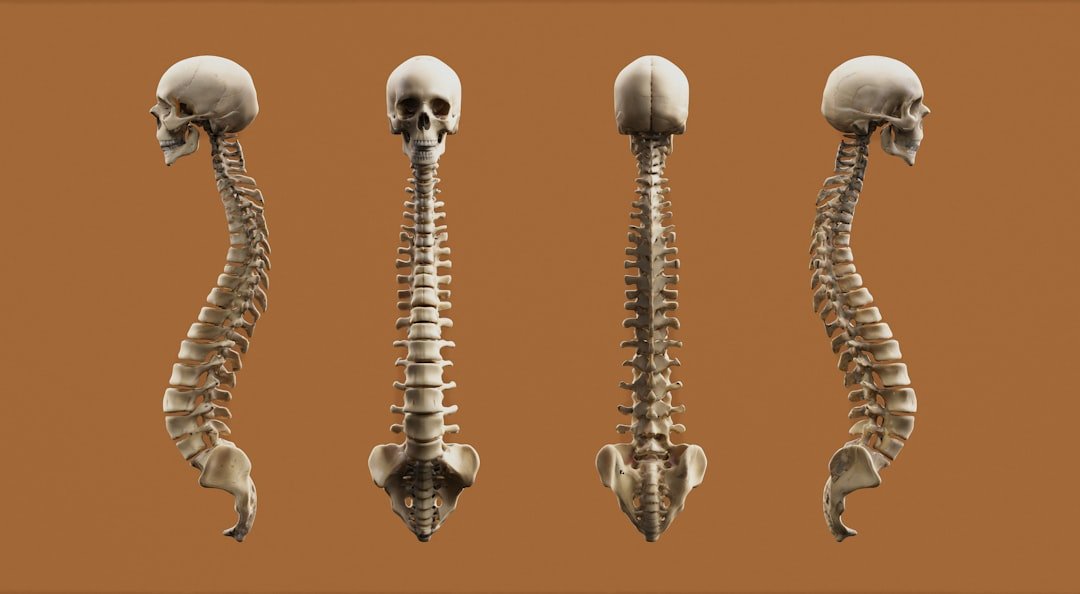
Minimally invasive techniques can address a wide range of spinal conditions affecting the cervical (neck), thoracic (upper back), and lumbar (lower back) regions. The goal is often to decompress nerves, stabilize the spine, or both.
Lumbar Spine Conditions
The lower back is a common site for spinal issues, and many can be treated minimally invasively:
- Herniated Discs: When the soft cushioning disc between vertebrae bulges or ruptures, it can press on nearby nerves. Minimally invasive discectomy can remove the offending disc material.
- Spinal Stenosis: This condition involves a narrowing of the spinal canal, often due to bone spurs or thickened ligaments, which can compress the spinal cord or nerves. Minimally invasive decompression techniques, such as laminotomy or foraminotomy, can relieve this pressure. Ultrasonic decompressions, a specialized minimally invasive technique, can precisely remove bone with minimal impact on surrounding soft tissues.
- Degenerative Disc Disease: As discs wear down, they can cause pain and instability. Minimally invasive fusions (like those using ProneTransPsoas or PTP techniques) or even disc replacements can address these issues. PTP is an innovative technique that accesses the spine through a small incision in the side, avoiding major abdominal muscles and structures, which can be highly beneficial for patients.
- Spondylolisthesis: This occurs when one vertebra slips forward over another. Minimally invasive fusion can stabilize the affected segment.
Cervical and Thoracic Spine Conditions
While less common than lumbar issues, problems in the neck and upper back can also be addressed using MISS:
- Cervical Disc Herniation: Similar to the lumbar spine, a herniated disc in the neck can cause arm pain, numbness, or weakness. Minimally invasive discectomy and fusion (ACDF) or cervical disc replacement can be performed.
- Cervical Stenosis: Narrowing of the spinal canal in the neck can lead to myelopathy (spinal cord compression). Minimally invasive procedures can decompress the spinal cord.
- Thoracic Disc Herniation: Although less frequent, herniated discs in the thoracic spine can also be debilitating and may be suitable for minimally invasive approaches in select cases.
- Minor Scoliosis Correction: While complex scoliosis often requires traditional open surgery, some less severe curves can be managed with minimally invasive techniques, particularly for pain management and stabilization.
- Trauma Follow-Up (Stabilization): Following certain spinal injuries, MISS can be used for stabilization and fusion, especially if a larger open approach is not necessary or desirable.
Who is a Good Candidate for Minimally Invasive Spine Surgery?
Determining candidacy for MISS is a careful process that involves a thorough evaluation of your medical history, symptoms, physical examination, and diagnostic imaging. It’s not a one-size-fits-all solution; think of it like finding the right key for a specific lock.
Factors Favoring MISS Candidacy
Several factors generally lean towards a patient being a good candidate for MISS:
- Clearly Defined Problem: The source of your pain and neurological symptoms should be clearly identified and localized. This means diagnostic imaging, such as an MRI, should show a distinct anatomical problem (e.g., a specific herniated disc, a localized area of stenosis, or a clearly unstable segment) that correlates with your symptoms. If the problem is diffuse or widespread, MISS might be less effective.
- Failure of Conservative Treatment: This is paramount. Before considering surgery, it’s essential to have exhausted non-surgical options for a reasonable period (typically 6-12 weeks). Conservative treatments might include physical therapy, medication, injections, and activity modification. Surgery is usually considered a last resort when these measures fail to provide adequate relief.
- Good Overall Health: Patients in generally good health, without severe underlying medical conditions that would increase surgical risks, are better candidates. This includes control of conditions like diabetes, heart disease, and high blood pressure.
- Realistic Expectations: Patients should have a clear understanding of the potential benefits and risks of MISS, as well as the expected recovery process. Surgery aims to improve symptoms and function, not necessarily to eliminate all pain.
- Appropriate Body Mass Index (BMI): While MISS can sometimes be an option for individuals with higher BMIs who might be at increased risk for complications with open surgery, extreme obesity can still pose challenges for any surgical approach. Your surgeon will discuss this with you.
- Specific Spinal Conditions: As outlined above, certain conditions are particularly well-suited for minimally invasive techniques.
Factors That Might Rule Out MISS or Favor Traditional Surgery
Just as some factors favor MISS, others might indicate that traditional open surgery is a more appropriate or safer option:
- Complex Spinal Deformities: Severe scoliosis, kyphosis, or other complex deformities often require a more extensive open approach to achieve the necessary correction and fusion.
- Extensive Spinal Trauma: Major fractures, dislocations, or significant instability from trauma might necessitate a more robust, open approach for complete reconstruction and stabilization.
- Large Tumors or Infections: These conditions may require wider exposure to safely remove diseased tissue and ensure complete treatment.
- Previous Extensive Spinal Surgery: Scar tissue from prior surgeries can make minimally invasive approaches more challenging or risky.
- Significant Instability in Multiple Segments: If instability spans several vertebral levels, an open approach might be preferred to achieve comprehensive fusion.
- Lack of a Clear Surgical Target: If diagnostic findings don’t precisely identify the anatomical source of pain, surgery of any kind, including MISS, may not be recommended.
- Certain Anatomical Considerations: Unique patient anatomy or technical difficulties identified during pre-operative planning might lead the surgeon to opt for an open approach.
The Diagnostic Process: Uncovering the Root Cause
Before any surgical consideration, a thorough diagnostic process is essential. This is like assembling a puzzle; each piece helps the surgeon see the full picture of your spinal health.
Initial Consultation and Physical Exam
Your journey typically begins with a detailed discussion of your medical history, including the onset, nature, and severity of your symptoms (pain, numbness, weakness, etc.). The surgeon will also perform a comprehensive physical examination to assess:
- Range of motion: How well you can move your spine.
- Neurological function: Checking reflexes, muscle strength, and sensation in your arms and legs.
- Pain reproduction: Special tests might be performed to see if certain movements reproduce your symptoms, helping to pinpoint the affected area.
Imaging Studies: X-rays and MRI
Imaging studies are critical for visualizing the spinal structures.
- X-rays: These provide images of bones and can reveal issues like spinal alignment problems (scoliosis, kyphosis), fractures, bone spurs, and signs of arthritis or instability. X-rays are often performed standing or bending to assess dynamic stability.
- MRI (Magnetic Resonance Imaging): This is the gold standard for visualizing soft tissues like discs, nerves, and the spinal cord. An MRI can clearly show herniated discs, spinal stenosis, nerve compression, tumors, and infections. This detailed view is crucial for planning minimally invasive procedures, as it allows the surgeon to identify the precise target for intervention. Dr. Moore offers a FREE MRI review/2nd opinion, which can be invaluable in understanding your imaging results and treatment options.
Other Diagnostic Tools
Sometimes, additional tests may be used:
- CT Scan (Computed Tomography): Provides more detailed images of bone than X-rays and can be useful for assessing complex fractures or bony anatomy.
- Nerve Conduction Studies (NCS) and Electromyography (EMG): These tests assess nerve function and muscle response, helping to confirm nerve compression and distinguish between nerve damage and other causes of pain.
- Diagnostic Injections: In some cases, a targeted injection of anesthetic into a specific area of the spine can temporarily relieve pain. If the pain resolves, it helps confirm that the injected area is indeed the source of the discomfort.
Minimally invasive spine surgery has gained popularity due to its potential benefits, but determining who is a good candidate for this procedure can be complex. For those interested in learning more about the criteria and considerations involved in this decision-making process, a related article can provide valuable insights. You can explore further details and schedule an appointment by visiting this link, which outlines the essential factors that influence candidacy for minimally invasive techniques.
Treatment Paths: From Conservative Care to Intervention
| Criteria | Description | Typical Patient Profile | Expected Benefits |
|---|---|---|---|
| Age | Generally suitable for adults of various ages, with consideration of overall health | Adults 30-70 years old | Reduced recovery time and less postoperative pain |
| Condition Type | Conditions treatable with minimally invasive techniques | Herniated discs, spinal stenosis, degenerative disc disease | Smaller incisions, less muscle damage |
| Overall Health | Patients without severe comorbidities that increase surgical risk | Non-smokers or controlled smokers, no severe heart or lung disease | Lower complication rates |
| Previous Spine Surgery | May be considered if no extensive scar tissue or anatomical changes | Patients with no or limited prior spine surgeries | Potential for quicker recovery compared to open revision surgery |
| Body Mass Index (BMI) | Lower BMI preferred for better surgical outcomes | BMI under 35 | Reduced risk of wound complications |
| Symptom Severity | Moderate to severe symptoms not responding to conservative treatment | Patients with persistent pain, numbness, or weakness | Improved function and pain relief |
The decision to pursue surgery, even minimally invasive, is a significant one and is always approached as part of a step-wise treatment plan.
Conservative Care First
As mentioned, surgery is typically considered after a trial of conservative care has failed to provide sufficient relief. This initial phase often includes:
- Rest and Activity Modification: Avoiding activities that aggravate your symptoms.
- Physical Therapy: Strengthening exercises, stretching, and modalities like heat/cold therapy to improve spinal function and reduce pain.
- Medications: Over-the-counter pain relievers, anti-inflammatory drugs, muscle relaxants, or neuropathic pain medications.
- Steroid Injections: Epidural steroid injections can reduce inflammation and provide temporary pain relief.
- Chiropractic Care or Acupuncture: Some patients find relief through these alternative therapies.
The goal of conservative care is to empower your body to heal itself and manage symptoms without surgical intervention.
When Surgery Becomes an Option
If conservative treatments don’t resolve your symptoms, and your quality of life remains significantly impaired, your surgeon may discuss surgical options. The choice between minimally invasive and traditional open surgery will depend on all the factors discussed previously.
Dr. Moore specializes in a range of minimally invasive approaches, including:
- ProneTransPsoas (PTP) Technique: A cutting-edge lateral approach for lumbar fusion that minimizes muscle disruption by going through the side of the body.
- Ultrasonic Decompressions: Use of high-frequency vibrations to precisely remove bone and other tissues causing nerve compression, enhancing precision and minimizing surrounding tissue damage.
- Minimally Invasive Discectomy: Removal of herniated disc material.
- Minimally Invasive Laminectomy/Foraminotomy: Decompression of nerves.
- Minimally Invasive Fusion: Stabilizing unstable spinal segments.
- Cervical Disc Replacement: Replacing a damaged disc in the neck with an artificial one to preserve motion.
- Scoliosis Correction (select cases): Addressing spinal curvature with less invasive methods.
- Trauma Follow-up: Stabilizing the spine after certain injuries.
The decision for surgery is a collaborative one between you and your surgeon, considering your specific condition, overall health, and personal preferences.
Minimally invasive spine surgery has gained popularity due to its potential benefits, but determining who is a good candidate for the procedure can be complex. For those interested in exploring this topic further, a related article discusses essential studies that shed light on various spine and orthopedic conditions. You can read more about these findings in the article available here, providing valuable insights that may help patients and healthcare providers make informed decisions regarding treatment options.
Important Safety Information and Next Steps
Your spinal health is precious. While minimally invasive spine surgery offers many advantages, it’s vital to be aware of potential warning signs and to seek professional medical advice.
Safety Red Flags to Watch For
While most back pain is not an emergency, certain symptoms warrant immediate medical attention. These “red flags” can indicate a more serious condition:
- New or worsening weakness in your legs or arms: Difficulty lifting your foot, holding objects, or unexplained clumsiness.
- Loss of bowel or bladder control: Incontinence or difficulty urinating/defecating. This is a medical emergency known as Cauda Equina Syndrome.
- Severe, unremitting back pain that does not improve with rest: Pain that keeps you awake at night.
- Unexplained weight loss or fever accompanied by back pain: These could indicate an infection or tumor.
- Back pain following a significant injury or trauma: Especially if accompanied by numbness or weakness.
Seek Qualified Medical Advice
It is essential to consult with a fellowship-trained orthopedic spine surgeon for an accurate diagnosis and appropriate treatment plan. Self-diagnosis and relying solely on online information can be misleading and potentially harmful. A specialist like Dr. Jeffrey Moore has the expertise and experience to differentiate between various spinal conditions and recommend the most effective and safest treatment approach for your unique situation.
If you are experiencing back or neck pain, or if you have been previously diagnosed with a spinal condition and are exploring your options, we encourage you to take the next step.
Call (405) 645-5475 to schedule a consultation or book online at JeffreyMooreSpine.com.
We also offer a FREE MRI review/2nd opinion, providing you with expert insight into your imaging and potential treatment paths.
FAQs
What is minimally invasive spine surgery?
Minimally invasive spine surgery (MISS) is a type of surgical procedure that uses smaller incisions and specialized instruments to access the spine. This approach aims to reduce tissue damage, minimize pain, and shorten recovery time compared to traditional open spine surgery.
Who is considered a good candidate for minimally invasive spine surgery?
Good candidates for MISS typically include patients with certain spinal conditions such as herniated discs, spinal stenosis, degenerative disc disease, or spinal instability who have not responded well to conservative treatments like physical therapy or medication. Candidates should be in generally good health and have a clear diagnosis that can be addressed with minimally invasive techniques.
Are there any conditions that might exclude someone from being a candidate for MISS?
Yes, patients with severe spinal deformities, extensive scar tissue from previous surgeries, infections, or certain complex spinal conditions may not be suitable candidates for minimally invasive spine surgery. The decision depends on individual medical evaluation by a spine specialist.
What are the benefits of minimally invasive spine surgery compared to traditional surgery?
Benefits of MISS include smaller incisions, less muscle and tissue damage, reduced blood loss, decreased postoperative pain, shorter hospital stays, faster recovery times, and lower risk of infection.
How is the candidacy for minimally invasive spine surgery determined?
Candidacy is determined through a comprehensive evaluation including medical history, physical examination, imaging studies (such as MRI or CT scans), and assessment of symptoms. A spine surgeon will evaluate whether MISS is appropriate based on the patient’s specific condition and overall health.
Can minimally invasive spine surgery be used for all types of spine problems?
No, MISS is not suitable for all spine problems. It is most effective for certain conditions like herniated discs, spinal stenosis, and some cases of spinal instability. Complex spinal deformities or tumors may require traditional open surgery.
What should patients expect during recovery from minimally invasive spine surgery?
Recovery from MISS is generally quicker than traditional surgery. Patients may experience less pain and can often return to normal activities sooner. However, recovery time varies depending on the specific procedure and individual health factors.
Is minimally invasive spine surgery safe?
When performed by an experienced spine surgeon, MISS is considered safe and effective. Like all surgeries, it carries some risks such as infection, bleeding, or nerve injury, but these risks are typically lower compared to open surgery.
How can I find out if I am a good candidate for minimally invasive spine surgery?
Consulting with a qualified spine specialist or neurosurgeon is the best way to determine candidacy. They will review your medical history, perform necessary tests, and discuss treatment options tailored to your condition.